Introduction: The history of medicine is replete with clinical practices, some clearly dangerous that have not been supported by what we would now consider to be mandatory data. Likewise, the field of hematology has not been immune from such practices as, for example, routine laparotomy and splenectomy in Hodgkin disease. Despite such history, and a push for evidence-based medicine, contemporary patient care still includes practices that have mainstream support despite a dearth of supporting evidence. CNS prophylaxis for diffuse large B-cell lymphoma(DLBCL) is one glaring example.
Current Practice: In patients with high CNS-IPI score (≥4), multiple extra-nodal (EN) sites (≥3) and high-risk extra-nodal site, brain imaging is obtained (usually MRI) and cerebro-spinal fluid (CSF) is analyzed. If CNS involvement at diagnosis is ruled out, systemic chemotherapy followed by high-dose methotrexate (HD-MTX) is typically offered to fit patients. Intra-thecal (IT) therapy or no prophylaxis is the usual practice for unfit patients. These therapies, modelled on the CNS prophylaxis in adults with acute lymphoblastic leukemia (ALL), are not free of side effects and include mucositis, myelosuppression, hepatic, renal, neurological, and gastro-intestinal toxicities.
Expert Opinion: Multiple national guidelines support the use of CNS prophylaxis for high-risk DLBCL. For example, the updated NCCN guidelines state that “CNS prophylaxis should be considered for patients with risk factors for CNS disease, but the optimal method is controversial”( NCCN Guidelines®, B cell lymphomas, version 5.2023). The British Society of Haematology recommend HD MTX administration for “high risk patients that are considered fit for such treatment”(McKay et al. British Journal of Haematology 2020). The European Society for Medical Oncology (ESMO) states that “HD-MTX is an option, even though the level of supporting evidence is low”(Tilly et al. Annals of Oncology 2015) ; the Canadian Lymphoma group recommends that ' Patients at high risk 'could consider' prophylaxis with high dose methotrexate“( Shafey et al. 2021) ; the Spanish Lymphoma Group recommends that 'CNS-directed prophylaxis should be offered to patients at high risk of CNS relapse'(Peñalver et al. Haematologica 2017). Similarly , multiple 'How I Treat' or guideline articles in top journals( Melchardt et al. ESMO Open 2023; Peñalver et al. Haematologica 2017; Bobillo et al. Haematologica 2023) support such use.
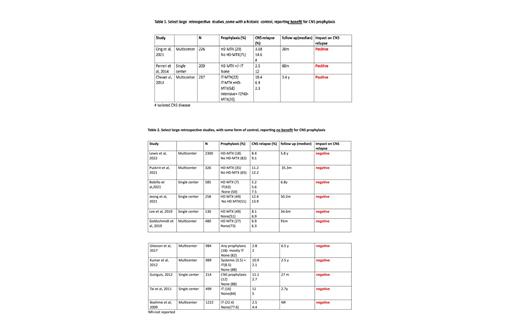
Published data: There are no randomized controlled studies assessing CNS prophylaxis compared to none. There are, however, multiple reports in the past two decades of the use of some form of CNS prophylaxis. Without any controls, the value of such therapy is impossible to assess. At the same time, there are several comparative reports, based only on historic controls and compounded by heterogeneity of treatments and comorbidities, that suggested a benefit for CNS prophylaxis (Table 1). More recently, a large body of retrospective studies, with controls, were published (Table 2). These included a cohort that received HD-MTX versus those who did not receive HD-MTX or those who did not receive any CNS prophylaxis. In virtually all these reports there was no evidence of reduction in CNS relapse.
Widespread use: Currently, the use of CNS prophylaxis is prevalent among fit and young patients with high-risk features ( Bobillo et al. Haematologica 2023; Demirci et al. Blood Research 2023). The concern for CNS relapse is the driving force behind this practice with a muted assurance that such may indeed prevent disease recurrence. Among older or unfit patients, CNS prophylaxis is most often withheld, with no evidence of a higher rate of CNS relapse ( Boehme et al. Blood, 2009; Eyre et al. Haematologica 2019).
Conclusion: Relapse in the CNS after treatment of DLBCL has long been recognized as a serious clinical problem. It was assumed by many that, as in ALL, simple prophylaxis would be an effective remedy. This hope was never convincingly shown to be effective. Several phase II studies, with biased controls, suggested a benefit which, nevertheless, could not be confirmed in large retrospective controlled studies. Perhaps a different mold of CNS prophylaxis is needed, but the current approach appears marginally effective at best or unnecessarily harmful, at worst. Is it not time to step forward and resolve this issue, before it becomes religiously entrenched as standard of care?
Disclosures
No relevant conflicts of interest to declare.